Using such a structured approach offers several advantages. It facilitates a streamlined authorization process by providing insurers with the necessary information to assess the request efficiently. This can lead to faster approval times and quicker access to necessary care for patients. Furthermore, it promotes standardized communication, minimizing potential misunderstandings and ensuring all parties involved are informed about the rationale behind the requested medical services. Properly completed documentation also reduces the likelihood of claim denials, saving time and resources for both providers and patients.
This foundational understanding of structured justifications for medical services will prove valuable as we explore specific use cases, completion guidelines, and best practices in the sections that follow.
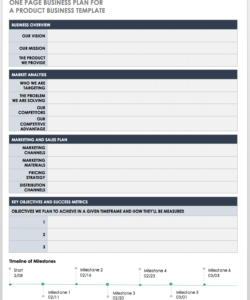
1. Standardized Format
Standardized formats are fundamental to the efficacy of medical necessity documentation. A consistent structure ensures all necessary information is presented clearly and logically, facilitating efficient review by insurers. This standardization minimizes ambiguity and reduces the likelihood of requests being denied due to missing or unclear information. A standardized template typically includes sections for patient demographics, relevant diagnoses, proposed treatments, and supporting clinical evidence. This structured approach enables payers to quickly locate and assess the critical information needed for informed decision-making.
Consider a scenario where multiple healthcare providers submit documentation with varying formats and levels of detail. This inconsistency can lead to significant processing delays as insurers struggle to extract the required information. In contrast, a standardized format ensures uniformity, allowing for streamlined review and quicker decision-making. For instance, using consistent terminology for diagnoses and procedures simplifies coding and reduces the potential for misinterpretation. Moreover, a standardized format promotes transparency and accountability by providing a clear audit trail of the decision-making process.
Standardization in medical necessity documentation is critical for efficient healthcare administration. It reduces processing times, improves communication between providers and payers, and ultimately contributes to better patient outcomes. While specific requirements may vary between payers and jurisdictions, adherence to established guidelines for formatting and content remains crucial for successful claim submissions and timely access to necessary medical services. This foundational element ensures a clear and consistent process, ultimately benefiting both patients and the healthcare system.
2. Patient Demographics
Accurate patient demographics are essential within a medical necessity template. These identifiers establish the individual for whom the services are requested and provide context for the medical necessity review. Demographics typically include the patient’s full name, date of birth, gender, address, and contact information. These data points ensure correct identification and facilitate communication regarding the request. Accurate demographics are crucial for avoiding delays or denials due to mismatched information. For example, an incorrect date of birth could lead to a claim denial or delay in processing, highlighting the importance of verifying all demographic details.
Beyond basic identification, patient demographics contribute to a more complete understanding of the individual’s medical needs. Factors such as age and gender can influence treatment decisions and play a role in determining medical necessity. Certain conditions are more prevalent in specific age groups or genders. This contextual information enhances the reviewer’s understanding of the case and supports the justification for the requested services. For instance, a medical necessity request for a bone density scan might be supported by the patient’s age and gender if those factors place them at higher risk for osteoporosis.
In conclusion, accurate and complete patient demographics are integral to a successful medical necessity submission. They ensure proper identification, facilitate communication, and provide valuable context for evaluating the medical necessity of requested services. Careful attention to detail in this area minimizes processing delays, reduces administrative burden, and ultimately contributes to timely and appropriate patient care. These data points are not merely administrative details but rather fundamental components of a comprehensive and effective request for necessary medical services.
3. Diagnosis Information
Diagnosis information forms the cornerstone of a statement of medical necessity template. A clear, concise, and accurate diagnosis establishes the medical rationale for the requested services or equipment. This information directly links the patient’s condition to the need for the specific intervention, providing the fundamental justification for approval. The diagnosis must be supported by appropriate clinical documentation, such as laboratory results, imaging reports, or specialist consultations. For instance, a diagnosis of type 2 diabetes mellitus substantiates a request for diabetic supplies and medication, while a diagnosis of osteoarthritis might justify the need for physical therapy or joint replacement surgery. Without a clearly stated and documented diagnosis, the request lacks the necessary foundation for approval.
The specificity and completeness of the diagnosis information are crucial. A general diagnosis might not adequately justify the requested service. For example, simply stating “back pain” is less compelling than specifying “lumbar spinal stenosis with radiculopathy.” The more precise the diagnosis, the clearer the medical necessity becomes. Further, including relevant diagnostic codes, such as ICD-10 codes, ensures standardized communication and facilitates efficient processing. These codes provide a universally understood language for describing medical conditions, streamlining the review process. A well-defined diagnosis, supported by relevant codes and clinical documentation, strengthens the justification and increases the likelihood of approval.
In summary, robust diagnosis information is paramount for a successful medical necessity request. It provides the essential link between the patient’s condition and the requested services, forming the core justification for approval. Clear, concise, and specific diagnoses, supported by relevant documentation and coding, ensure efficient processing, reduce the likelihood of denials, and ultimately contribute to timely access to necessary medical care. The accuracy and completeness of this information directly impact the outcome of the request and underscore its critical role in the overall process.
4. Treatment Rationale
The treatment rationale within a statement of medical necessity template provides the critical link between the diagnosed condition and the proposed treatment plan. It explains why the specific treatment or intervention is necessary and appropriate for the patient’s particular circumstances. This justification often involves detailing the expected benefits of the treatment, outlining how it will address the patient’s symptoms or improve their condition. A robust treatment rationale draws upon established medical guidelines, research findings, and clinical experience to support the proposed approach. For example, if a patient with a herniated disc is recommended for physical therapy, the rationale might explain how targeted exercises can strengthen supporting muscles, improve mobility, and reduce pain. Conversely, if surgery is proposed, the rationale might describe the severity of the herniation, the failure of conservative treatments, and the expected benefits of surgical intervention in alleviating nerve compression. Without a compelling treatment rationale, the medical necessity request lacks the crucial justification for approval.
Furthermore, the treatment rationale should address alternative treatment options considered and explain why they were deemed less suitable. This demonstration of due diligence strengthens the argument for the proposed treatment and provides a comprehensive view of the decision-making process. For instance, if a patient is recommended for a brand-name medication, the rationale should explain why a less expensive generic alternative is not appropriate, perhaps due to specific patient allergies or documented ineffectiveness of the generic option in the past. This comparative analysis adds weight to the justification and demonstrates a thoughtful approach to patient care. In addition, the treatment rationale may incorporate a prognosis, outlining the expected outcomes with and without the proposed intervention. This projection helps to clarify the potential benefits of the treatment and further underscores its medical necessity.
In conclusion, the treatment rationale serves as a pivotal element within the medical necessity template. It provides the essential justification for the proposed treatment plan, linking it directly to the patient’s diagnosed condition and expected outcomes. A well-constructed rationale incorporates evidence-based medicine, addresses alternative options, and offers a clear prognosis, strengthening the request and increasing the likelihood of approval. This component is not merely a formality but rather a crucial element that ensures patients receive appropriate and medically necessary care. Its clarity and comprehensiveness directly impact the effectiveness and efficiency of the healthcare delivery process.
5. Supporting Evidence
Supporting evidence forms the bedrock of a credible statement of medical necessity template. It transforms assertions of medical need into substantiated justifications, increasing the likelihood of approval for requested services or equipment. Robust supporting evidence provides objective data and clinical findings that validate the stated diagnosis and treatment rationale. This evidence bridges the gap between clinical judgment and payer requirements, ensuring a transparent and defensible request.
- Clinical Findings:Objective clinical findings documented in patient records serve as primary supporting evidence. These findings might include physical examination results, vital signs, laboratory test results, imaging reports (X-rays, MRIs, CT scans), and documented symptoms. For example, elevated blood glucose levels support a diabetes diagnosis, while an MRI showing spinal stenosis corroborates the need for back surgery. These concrete data points provide tangible proof of the patient’s condition and its severity, directly supporting the medical necessity argument.
- Prior Treatment History:Documentation of prior treatments, including their outcomes and duration, adds crucial context to the medical necessity argument. If previous conservative treatments have failed to alleviate the patient’s condition, this supports the need for more intensive interventions. For instance, documented failure of physical therapy and pain management for a knee injury strengthens the justification for knee replacement surgery. This history demonstrates that less invasive options have been explored and proven ineffective, underscoring the necessity of the proposed treatment.
- Specialist Consultations:Reports from specialist consultations provide expert opinions that can significantly bolster a medical necessity request. These reports often offer in-depth analyses of the patient’s condition, confirming the diagnosis and supporting the proposed treatment plan. A cardiologist’s recommendation for cardiac catheterization, for example, carries significant weight in justifying the procedure’s medical necessity. Specialist input adds a layer of authoritative support, validating the referring physician’s assessment and strengthening the overall request.
- Peer-Reviewed Literature:Citing relevant peer-reviewed literature, especially established clinical guidelines, adds further credibility to the medical necessity argument. These sources provide evidence-based support for the proposed treatment, demonstrating that it aligns with accepted standards of care within the medical community. Referencing guidelines for managing specific conditions demonstrates a commitment to best practices and strengthens the justification for the requested services. This evidence-based approach ensures the proposed treatment is not only medically sound but also supported by current scientific understanding.
The convergence of these supporting evidence components creates a compelling case for medical necessity. By providing objective data, clinical findings, and expert opinions, the supporting evidence strengthens the request, increasing the likelihood of approval and ensuring patients receive the appropriate care they need. A well-supported medical necessity request reflects a thorough and thoughtful approach to patient care, ultimately benefiting both the patient and the healthcare system as a whole.
6. Provider Signature
The provider’s signature on a statement of medical necessity template serves as a critical element, signifying professional accountability and validating the information contained within the document. It attests to the provider’s belief that the requested services or equipment are medically necessary for the patient’s well-being, based on their professional judgment and clinical evaluation. This signature transforms the document from a collection of data into a formal request, carrying the weight of the provider’s expertise and licensure. Without a valid provider signature, the document lacks the necessary authority and may be deemed incomplete or invalid.
- Licensure Verification:The provider signature allows for verification of the individual’s licensure and credentials, ensuring they are qualified and authorized to order the requested services. This verification process protects patients by ensuring they receive care from appropriately licensed professionals. It also safeguards against fraudulent requests and maintains the integrity of the healthcare system. A signature linked to a verifiable license number provides an essential layer of accountability.
- Legal and Ethical Responsibility:The act of signing the document signifies the provider’s legal and ethical responsibility for the information provided. They attest to the accuracy and completeness of the information, acknowledging that the request is based on sound clinical judgment and adheres to professional standards of care. This accountability underscores the importance of the provider’s role in ensuring appropriate utilization of healthcare resources.
- Authentication and Non-Repudiation:The provider’s signature serves as a form of authentication, confirming the document’s origin and preventing its subsequent denial. This non-repudiation aspect is crucial for maintaining the integrity of the medical record and ensuring clear communication between healthcare providers and payers. It prevents disputes over authorship and reinforces the validity of the request.
- Formal Authorization:The signature formally authorizes the request for the specified services or equipment. It signifies the provider’s professional endorsement of the treatment plan, transforming the document into an actionable request for necessary healthcare resources. This authorization is crucial for initiating the approval process and ensuring timely access to care. Without the provider’s signature, the request remains incomplete and cannot be processed.
In the context of a statement of medical necessity template, the provider’s signature serves as the culminating act, transforming a collection of information into a validated, actionable request. It signifies professional accountability, confirms the accuracy of the information, and authorizes the requested services. This critical component underscores the provider’s central role in ensuring patients receive appropriate and medically necessary care, while simultaneously maintaining the integrity and efficiency of the healthcare system. A valid provider signature is essential for a complete and effective medical necessity request.
Key Components of a Medical Necessity Statement
A comprehensive medical necessity statement requires several key components to effectively communicate the patient’s need for specific services or equipment. These components ensure clarity, facilitate efficient processing, and contribute to a successful justification of the requested healthcare resources.
1. Patient Demographics: Accurate and complete patient demographics are essential for proper identification and contextualization of the medical necessity. These typically include full name, date of birth, gender, address, and contact information. Accurate demographics ensure efficient processing and minimize the risk of delays or denials.
2. Diagnosis Information: A clear, concise, and specific diagnosis establishes the medical rationale for the requested services. Supporting clinical documentation, including diagnostic codes (e.g., ICD-10 codes), strengthens the link between the patient’s condition and the need for the requested intervention.
3. Treatment Rationale: A robust treatment rationale explains why the proposed treatment or intervention is necessary and appropriate for the patient’s specific situation. This includes outlining the expected benefits, addressing alternative treatment options, and incorporating a prognosis.
4. Supporting Evidence: Objective data and clinical findings validate the stated diagnosis and treatment rationale. This evidence includes clinical findings, prior treatment history, specialist consultations, and relevant peer-reviewed literature. Strong supporting evidence substantiates the medical necessity argument.
5. Provider Signature: The provider’s signature validates the information within the document, attesting to its accuracy and the provider’s professional judgment. This signature signifies legal and ethical responsibility for the request and authorizes the provision of the specified services.
These interconnected components form a cohesive and persuasive argument for medical necessity. Each element plays a crucial role in ensuring that patients receive appropriate and timely access to essential healthcare resources. A thorough and well-structured medical necessity statement facilitates efficient processing, reduces the likelihood of denials, and ultimately contributes to better patient outcomes.
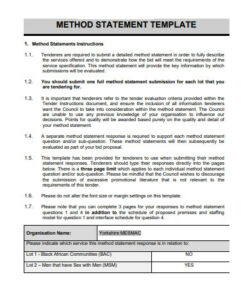
How to Create a Statement of Medical Necessity
Creating a comprehensive and effective statement of medical necessity requires careful attention to detail and a clear understanding of the required components. The following steps outline the process of developing a robust justification for requested medical services or equipment.
1. Gather Patient Information: Begin by collecting comprehensive patient demographics, including full name, date of birth, gender, contact information, and insurance details. Accurate patient information is crucial for proper identification and efficient processing.
2. Clearly State the Diagnosis: Provide a clear, concise, and specific diagnosis, supported by relevant ICD-10 codes. This diagnosis forms the foundation of the medical necessity argument, linking the patient’s condition to the requested services.
3. Describe the Proposed Treatment: Detail the proposed treatment or intervention, explaining the specific procedures, medications, or equipment requested. Clearly outline the anticipated benefits and the duration of the proposed treatment plan.
4. Provide a Compelling Treatment Rationale: Explain why the proposed treatment is medically necessary and appropriate for the patient’s specific circumstances. This rationale should draw upon established medical guidelines, research findings, and clinical experience. Address alternative treatment options considered and explain why they were deemed less suitable.
5. Include Supporting Evidence: Substantiate the medical necessity argument with objective data and clinical findings. Include relevant laboratory results, imaging reports, specialist consultations, prior treatment history, and citations from peer-reviewed literature, as appropriate. This evidence provides concrete support for the stated diagnosis and treatment rationale.
6. Obtain Provider Signature and Contact Information: Ensure the document includes the signature of the ordering provider, along with their contact information and credentials. This signature validates the information provided and authorizes the request. It also allows for verification of the provider’s licensure and facilitates communication if needed.
7. Review and Submit: Carefully review the completed statement of medical necessity for accuracy and completeness before submitting it to the relevant payer. Ensure all required fields are populated and all supporting documentation is included. A thorough review minimizes the risk of delays or denials.
A well-crafted statement of medical necessity clearly articulates the patient’s need for the requested services, providing a compelling justification based on medical evidence and clinical judgment. Adherence to these steps ensures a comprehensive and effective request, facilitating timely access to necessary medical care.
Precise and comprehensive documentation of medical necessity is paramount for ensuring patients receive appropriate and timely access to essential healthcare services. Understanding the core componentspatient demographics, accurate diagnoses, compelling treatment rationales, robust supporting evidence, and validated provider signaturesis fundamental for constructing effective justifications. Standardized templates offer a structured approach, promoting clarity and efficiency in communication between healthcare providers and payers. This meticulous approach to documentation not only facilitates the approval process but also contributes to better patient outcomes by ensuring access to necessary care.
Effective utilization of structured medical necessity documentation represents a crucial step towards optimizing healthcare resource allocation and improving the overall quality of patient care. As healthcare systems continue to evolve, the importance of clear, concise, and well-supported justifications for medical interventions will only continue to grow. Adherence to best practices in documentation ensures a transparent and accountable process, benefiting both individual patients and the healthcare system as a whole. This commitment to robust documentation ultimately fosters a more efficient and equitable healthcare landscape.