Navigating the complexities of healthcare can sometimes feel like a maze, both for patients and providers. At the heart of good practice lies clear, empathetic communication. It’s not just about delivering care; it’s about empowering individuals to understand their health journey and make informed decisions every step of the way. This foundation of trust and clarity is absolutely vital in any medical setting, from a small private clinic to a large hospital.
That’s where well-designed tools come into play, tools that bridge the communication gap and ensure everyone is on the same page. You might be wondering how to effectively achieve this consistency and professionalism without reinventing the wheel every time. The answer often lies in utilizing a robust patient information sheet and consent form template, which serves as a cornerstone for ethical practice and patient empowerment. These documents are more than just paperwork; they are essential instruments for transparency and mutual understanding in the healthcare environment.
Why A Comprehensive Patient Information Sheet Is Crucial
A patient information sheet, often abbreviated as PIS, is essentially a detailed guide designed to inform patients about a specific medical procedure, treatment, research study, or even the general services offered by a healthcare facility. Think of it as your patient’s personal handbook, providing all the necessary details in an easy-to-understand format. It goes beyond the brief verbal explanations, offering a tangible reference that patients can take home, review with family, and truly digest at their own pace.
For patients, a well-crafted PIS can significantly reduce anxiety and build confidence. When someone fully understands what to expect, from potential risks and benefits to alternative treatments and what post-care entails, they feel more in control and are better prepared for their experience. This proactive approach to information sharing fosters a sense of partnership between the patient and the healthcare provider, rather than a top-down instruction. It ensures that critical details aren’t lost in translation or forgotten moments after a consultation.
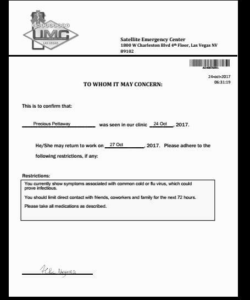
From the healthcare provider’s perspective, providing a comprehensive PIS isn’t just a courtesy; it’s often a regulatory requirement and a fundamental aspect of risk management. It demonstrates due diligence in informing patients and can serve as crucial documentation should any questions or disputes arise later. It standardizes the information delivery process, ensuring that every patient receives the same high quality of detail, regardless of who is explaining it.
Key Elements to Include in Your Patient Information Sheet
- **Contact Information:** Clear details for the clinic or department, including emergency contacts.
- **Description of Service/Procedure:** A plain language explanation of what will happen.
- **Purpose and Rationale:** Why this specific service or procedure is recommended.
- **Potential Benefits:** What the patient stands to gain.
- **Potential Risks and Side Effects:** A comprehensive, yet clear, list of potential downsides, complications, or discomforts.
- **Alternative Options:** Other available treatments or approaches, even if not offered by your facility.
- **What to Expect (Before, During, After):** Practical advice on preparation, the process itself, and recovery.
- **Confidentiality and Data Protection:** How their personal and medical information will be handled.
- **Right to Withdraw:** Confirmation that they can change their mind at any point before the procedure.
Moreover, a PIS can be incredibly useful for streamlining administrative processes. By answering common questions upfront, it can reduce the number of phone calls or follow-up queries, freeing up staff time and making the overall patient journey smoother for everyone involved. It’s an investment in efficiency and patient satisfaction.
The Indispensable Role of a Robust Consent Form
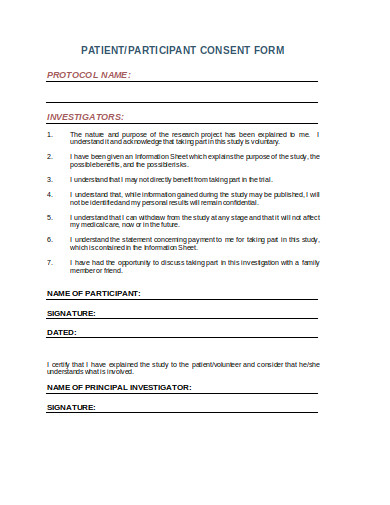
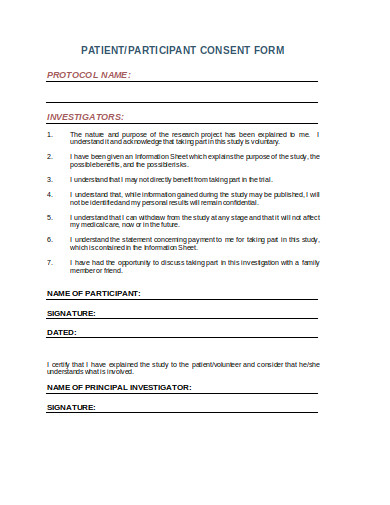
While the patient information sheet is about informing, the consent form is about formally acknowledging understanding and granting permission. Informed consent is a cornerstone of medical ethics and law, requiring that a patient has the capacity to make decisions, has been adequately informed, and has voluntarily agreed to a proposed medical intervention. A well-structured consent form provides documented proof that this vital process has occurred, protecting both the patient’s autonomy and the provider’s legal standing.
The journey to obtaining truly informed consent involves more than just a signature on a line. It begins with the information provided in the PIS and continues through a clear, verbal discussion where the patient has the opportunity to ask questions and receive satisfactory answers. The consent form then acts as the formal record that this dialogue has taken place and that the patient is willing to proceed based on the information they have received and understood.
Consent forms are crucial across a wide range of healthcare scenarios. They are indispensable for surgical procedures, invasive diagnostic tests, participation in clinical trials, the release of medical records, and even for basic patient registration where data handling and privacy policies are outlined. Without a solid consent form, healthcare providers face significant ethical dilemmas and potential legal liabilities, and patients may feel their rights are not fully respected.
A good consent form protects both the patient and the practitioner. For the patient, it ensures their rights are respected and that no procedure or treatment is undertaken without their explicit agreement. For the provider, it serves as legal evidence that appropriate steps were taken to inform the patient and secure their permission, helping to mitigate risks related to claims of negligence or assault. It underlines a commitment to patient-centered care and ethical practice.
To be effective, a consent form should always be written in clear, unambiguous language, avoiding medical jargon wherever possible. It should clearly state the name of the procedure or treatment, who will perform it, the risks and benefits, and any alternatives discussed. Crucially, it must also include a clear statement that the patient has had the opportunity to ask questions and that all queries have been answered to their satisfaction. Space for the patient’s signature, date, and sometimes a witness signature are standard components. A well-designed patient information sheet and consent form template ensures consistency and compliance, making the process smoother for everyone involved.
In essence, these documents are the twin pillars supporting transparent and ethical healthcare delivery. They empower individuals to be active participants in their care decisions and safeguard the integrity of the medical relationship. By investing time in creating clear, comprehensive, and legally sound documents, healthcare providers not only meet regulatory obligations but also foster a deeper level of trust and understanding with those they serve. They are invaluable tools for any practice committed to excellence and patient advocacy.