Navigating the complexities of patient care, especially in a specialized field like pain management, often requires seamless communication between medical professionals. When a patient needs to transition from one pain specialist to another, or even when a primary care physician refers them to a pain expert, having a clear and comprehensive system in place is absolutely vital. It’s not just about passing a name along; it’s about transferring a patient’s entire narrative, their unique pain journey, and all the critical medical details that will enable their new doctor to pick up precisely where the last left off, without missing a beat.
This is where a dedicated pain dr to pain dr refferal form template becomes an invaluable asset for any healthcare practice. Imagine the time saved, the reduction in administrative errors, and most importantly, the vastly improved patient experience when every piece of relevant information is neatly organized and easily accessible. Such a template ensures that the referring doctor provides exactly what the receiving doctor needs, fostering a collaborative environment that prioritizes continuity of care and optimal patient outcomes. It’s about creating a bridge of information that supports effective treatment strategies from day one.
Why a Specialized Pain Referral Form Matters
In the realm of pain management, patients often present with complex conditions that defy simple diagnoses. Their pain can be chronic, neuropathic, musculoskeletal, or a combination of many factors, influenced by previous injuries, surgeries, medications, and even psychological components. A generic referral form, designed for general medical consultations, simply cannot capture the nuances crucial for a pain specialist to effectively evaluate and treat a new patient. Without specific details regarding the pain’s onset, character, duration, alleviating and aggravating factors, or the outcomes of previous treatments, the receiving pain doctor has to start almost from scratch, potentially delaying appropriate care.
Think about the sheer volume of information that’s pertinent to a pain specialist. It goes far beyond basic demographics and a chief complaint. They need to understand the patient’s history of present illness in minute detail, including pain scales, mapping of pain areas, and what treatments have been tried and failed. They need comprehensive medication lists, including dosages and frequencies, along with any allergies or adverse reactions. Furthermore, an understanding of the patient’s psychosocial background, their coping mechanisms, and their functional limitations due to pain is often essential for crafting a holistic treatment plan.
For the referring doctor, using a specialized template simplifies the referral process significantly. Instead of trying to compile disparate notes or guess what information might be relevant, they have a clear, structured guide. This not only saves time but also instills confidence that they are providing a complete and helpful referral, ensuring their patient receives the best possible care from the outset. It streamlines their workflow and reduces follow-up calls or requests for additional information from the receiving end.
On the receiving end, the benefits are even more profound. A comprehensive pain dr to pain dr refferal form template allows the pain specialist to review the patient’s case thoroughly even before the initial consultation. This preparation can dramatically shorten the time needed for assessment, allowing the doctor to formulate more targeted questions, anticipate potential challenges, and even suggest preliminary diagnostic tests or treatment pathways. It means less time spent gathering basic information during the appointment and more time focusing on nuanced clinical decision-making, leading to quicker and more effective intervention for the patient.
Key Elements of an Effective Pain Referral Form
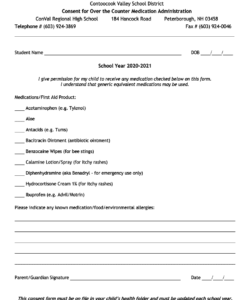
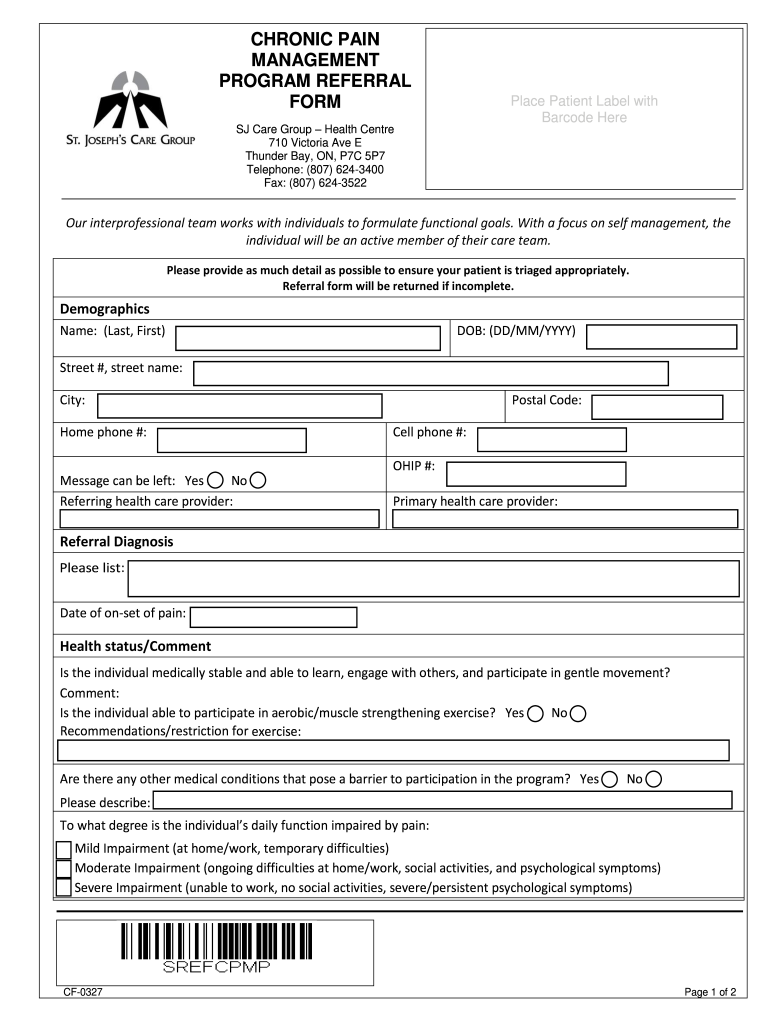
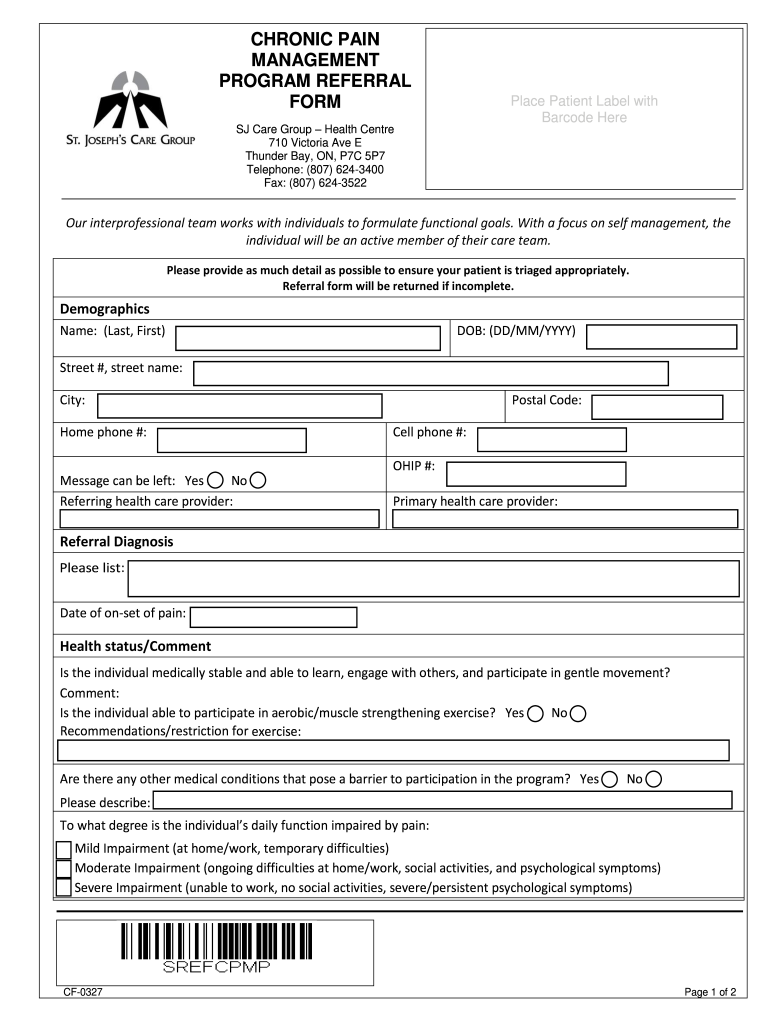
- Patient Demographics: Full name, date of birth, contact information, insurance details.
- Referring Physician Details: Name, practice, contact information, NPI.
- Reason for Referral: Clear, concise statement of the primary pain complaint.
- History of Present Illness: Onset, duration, location, character (e.g., sharp, burning, aching), severity (pain scale), aggravating/alleviating factors.
- Past Medical History: Relevant conditions, surgeries, injuries, and previous pain-related diagnoses.
- Current Medications: Full list of all prescriptions, over-the-counter drugs, and supplements, including dosages.
- Allergies: Documented allergies and reactions.
- Previous Pain Treatments and Outcomes: Details of past therapies (medications, injections, physical therapy, chiropractic care, etc.) and their effectiveness.
- Diagnostic Imaging and Labs: Relevant reports (MRI, X-ray, CT scans, blood tests) with dates and findings.
- Functional Impact: How pain affects daily activities, work, sleep, and quality of life.
- Psychosocial Factors: Any relevant mental health history, social support, or contributing stressors.
- Goals of Care: What the patient hopes to achieve from pain management.
Building Your Ideal Pain Dr to Pain Dr Refferal Form Template
Crafting a referral form that perfectly fits your practice’s needs and ensures robust communication takes a bit of thoughtful design. The best templates aren’t just generic forms; they are tailored instruments that reflect the specific information exchange most valuable to pain specialists. Start by collaborating with both the referring primary care providers and the pain specialists within your network or practice. Ask them what information they find most crucial when sending or receiving a patient with complex pain, and what details are often missing or unclear on existing forms. This collaborative approach ensures that the template is not only comprehensive but also practical and user-friendly for everyone involved in the patient’s care continuum.
When designing the layout, aim for clarity and logical flow. Group related information together, using clear headings and distinct sections. Employing checkboxes where appropriate can save time and reduce ambiguity, especially for common conditions or treatment modalities. However, also ensure there is ample space for narrative descriptions, allowing physicians to add critical context that might not fit into a pre-defined field. Remember, while efficiency is key, the human element of medicine—the detailed story of a patient’s struggle—must not be lost in the process.
Consider the format of your template. While paper forms are still common, many practices are moving towards digital solutions for their ease of use, accessibility, and enhanced security. Electronic templates can be integrated into Electronic Health Record (EHR) systems, allowing for seamless autofill of patient demographics and quick attachment of relevant medical records. If using a digital format, ensure it adheres to all privacy regulations, like HIPAA, to protect sensitive patient information during transmission. Security isn’t just a compliance issue; it’s a fundamental aspect of trust between patients, referring doctors, and specialists.
Finally, remember that your pain dr to pain dr refferal form template is not a static document. The landscape of pain management evolves, new treatments emerge, and best practices are refined over time. Schedule periodic reviews of your template, perhaps annually, to ensure it remains current, effective, and continues to meet the needs of all parties involved. Gathering feedback from both referring and receiving practitioners after implementation can provide valuable insights for continuous improvement, making your referral process even more efficient and patient-centered in the long run.
Streamlining the referral process for pain patients is a significant step towards improving healthcare delivery. By implementing a meticulously designed form, practices can ensure that patients receive timely, appropriate, and continuous care. This dedication to clear communication and detailed information sharing ultimately translates into better health outcomes and a more positive experience for individuals living with chronic pain, fostering a system where collaboration truly benefits the patient.