When a patient transitions from home health services back to self-management or another level of care, the process needs to be smooth and comprehensive. This isn’t just about saying goodbye; it’s about ensuring continuity of care and preventing readmissions. Effective discharge planning is a cornerstone of quality home health, guiding patients and their families through the next steps in their health journey.
That’s where a robust discharge form comes into play. It acts as a critical bridge, summarizing everything important a patient needs to know as they leave your direct care. Think of it as a roadmap for their ongoing well-being, designed to empower them with the information and resources necessary to maintain their health improvements and manage any lingering conditions effectively. It’s truly an indispensable tool for every home health agency.
The Essential Elements of a Comprehensive Home Health Discharge Form
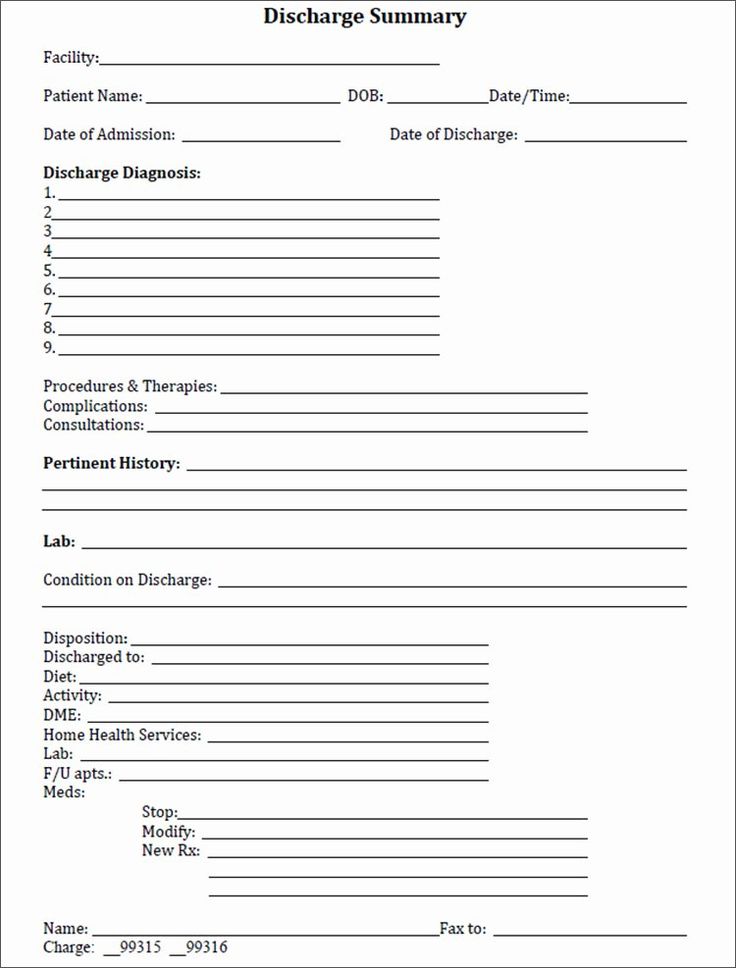
A well-designed home health discharge form template isn’t just a checklist; it’s a detailed record that encapsulates the entire care journey and sets the stage for future health management. The goal is to ensure nothing vital is overlooked, providing a clear, actionable plan for the patient and any subsequent caregivers. Starting with basic patient demographics, it branches out into highly specific medical information and follow-up instructions.
One of the most critical sections involves patient identification and contact details, alongside emergency contacts. This ensures that in any unforeseen circumstance, the patient or their designated support person can be reached. Equally important are the details of the home health agency and the primary care physician or specialist who will be assuming care. This facilitates smooth communication between providers, a key factor in preventing fragmented care.
Key Information to Include for Optimal Patient Transition
Beyond the basics, a truly effective form delves into the specifics of the care provided and the patient’s status at discharge. This typically includes a concise summary of the patient’s diagnosis and medical history relevant to the home health episode. Think about major health events, chronic conditions, and any acute issues addressed during their time under home health care. This context is vital for anyone taking over their care.
It also needs to clearly outline the services received, the duration of care, and the progress made towards established goals. This can be presented as:
- A summary of skilled nursing visits and interventions
- Details of therapy services (physical, occupational, speech) and their outcomes
- Information on any medical social work or home health aide services provided
Crucially, medication reconciliation is paramount. The form must list all current medications, including dosage, frequency, route, and clear instructions for administration, noting any changes made during home health care. It should also highlight medications to be discontinued and new prescriptions initiated. Patient education is another cornerstone; documenting what the patient and caregiver have been taught about their condition, medications, diet, and activity restrictions is essential for self-management and reinforces learned behaviors.
Benefits of Utilizing a Standardized Home Health Discharge Form Template
Implementing a standardized home health discharge form template brings a multitude of advantages to home health agencies, patients, and even the broader healthcare system. First and foremost, it ensures consistency and compliance across all discharge processes. Every patient receives the same high quality of information, formatted in an easily understandable way, reducing the risk of critical details being missed or miscommunicated. This uniformity is vital for regulatory adherence and helps maintain high standards of care.
From the patient’s perspective, a clear, standardized form significantly enhances their understanding and empowerment. When they receive consistent, well-organized instructions, they are far more likely to adhere to follow-up care plans, manage their medications correctly, and recognize warning signs that require immediate attention. This proactive approach to patient education directly contributes to improved health outcomes and fosters a sense of trust in their care providers.
For the home health agency, standardization streamlines administrative tasks and improves efficiency. Clinicians spend less time creating unique discharge summaries from scratch and more time focusing on direct patient care. Training new staff on discharge protocols becomes simpler, as there’s a clear, established framework to follow. This efficiency not only saves time but also reduces the potential for errors that can arise from ad-hoc documentation.
Furthermore, using a reliable home health discharge form template helps reduce readmission rates. By clearly outlining follow-up appointments, providing emergency contact information, and detailing potential complications, the form equips patients to avoid preventable hospital visits. It bridges the gap between acute care and ongoing self-management, fostering better continuity of care and contributing to a more sustainable healthcare model for everyone involved. It’s a proactive step towards better patient safety and operational excellence.
The moment a patient transitions out of home health care is just as vital as their admission. It’s an opportunity to solidify their progress, equip them with essential knowledge, and ensure a seamless continuation of their health journey. A thoughtfully prepared discharge document is not merely a formality; it is a critical tool for patient empowerment and a testament to the quality of care provided.
By investing in a comprehensive and easy-to-use home health discharge form, agencies can significantly enhance patient safety, improve outcomes, and streamline their internal processes. It’s about building a solid foundation for patients to maintain their well-being long after the home health team has departed, ensuring they feel confident and supported in their ongoing health management.