Navigating the complexities of healthcare, especially within the Medicaid system, requires meticulous attention to detail. For nursing professionals, accurate and comprehensive documentation isnt just a best practice; it is a fundamental requirement for ensuring patient safety, facilitating continuity of care, and securing appropriate reimbursement. The sheer volume of information that needs to be recorded, from daily assessments to medication administration and care plan updates, can be daunting. This is where a well-designed documentation system becomes indispensable, transforming a potentially overwhelming task into a streamlined process.
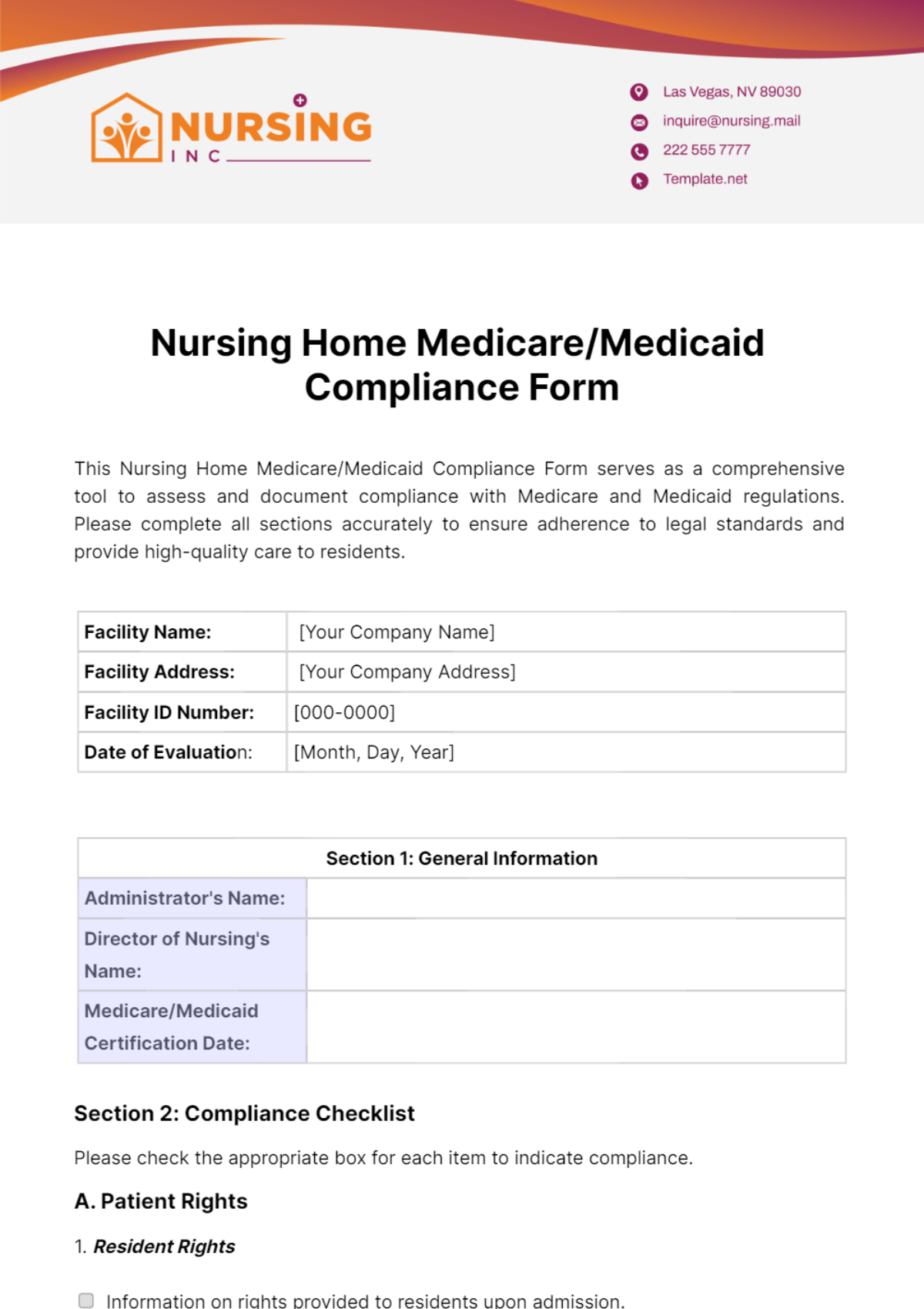
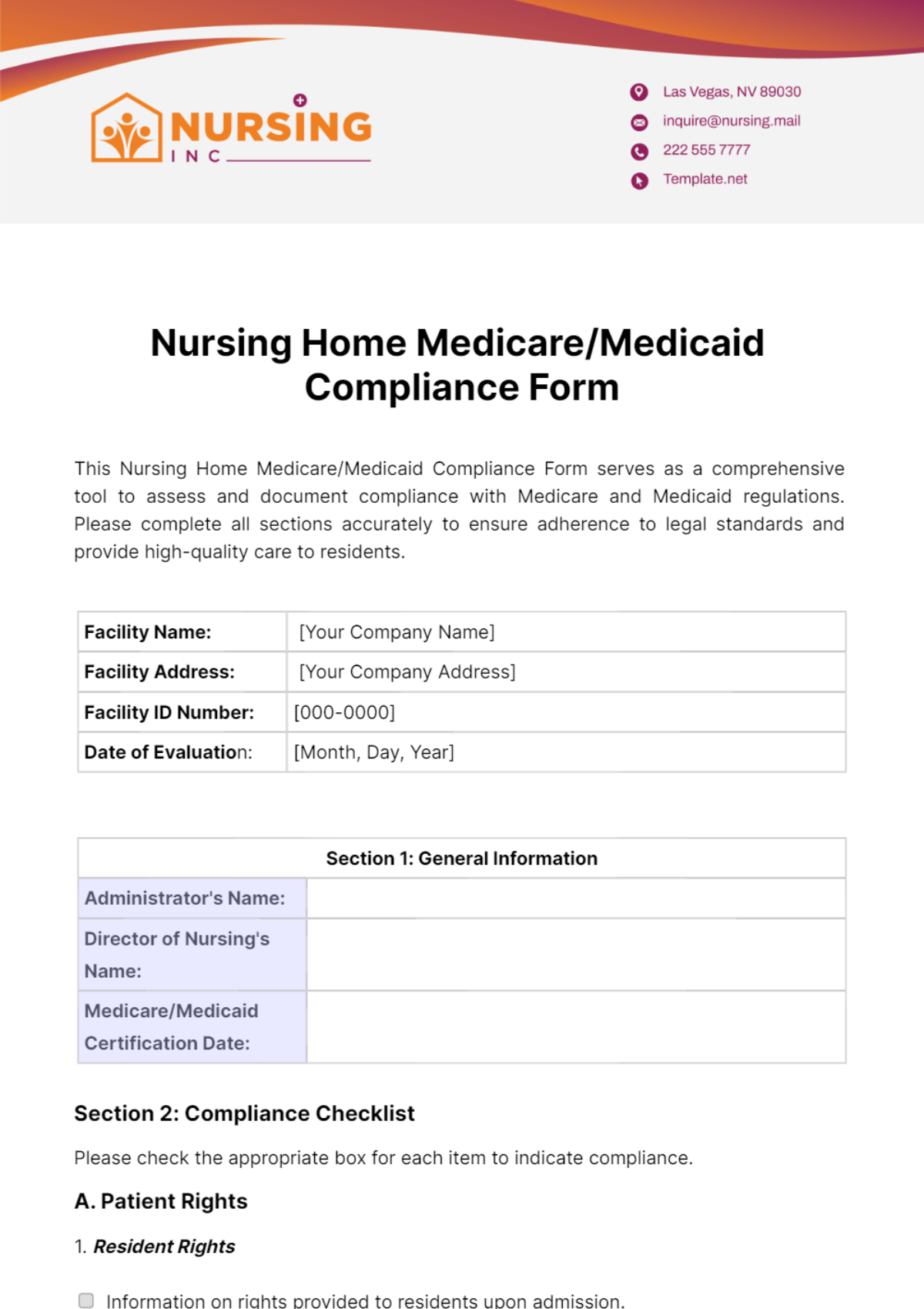
Implementing a standardized form, such as a robust medicaid nursing documentation form template, can significantly alleviate this burden. Such a template acts as a structured guide, ensuring that all necessary information is captured consistently and efficiently. It helps reduce errors, minimizes the risk of missing critical data, and provides a clear, defensible record of the care provided. For nurses, it means less time spent deciphering notes or trying to remember what to include, freeing up valuable time to focus on what truly matters: delivering exceptional patient care.
Why a Standardized Medicaid Nursing Documentation Form is Crucial
In the realm of Medicaid services, adherence to specific regulatory requirements is not merely suggested; it is mandated. State and federal regulations govern every aspect of care delivery and reimbursement, making precise documentation a cornerstone of compliance. Inaccurate or incomplete records can lead to denied claims, audits, and even legal ramifications for healthcare providers. A standardized medicaid nursing documentation form template ensures that every data point required for compliance, from the initial assessment to ongoing interventions and outcomes, is systematically collected and easily retrievable, protecting both the provider and the patient.
Beyond regulatory compliance, consistent documentation profoundly impacts the quality of patient care. When all nurses and care team members follow the same standardized format, it creates a cohesive and easily understood patient record. This seamless flow of information is vital for effective care coordination, especially when multiple providers are involved or when patients transition between different levels of care. It allows any healthcare professional to quickly grasp the patient’s history, current status, and care plan, minimizing miscommunication and enhancing patient safety.
Furthermore, a well-structured template significantly boosts efficiency within nursing operations. Imagine the time saved when nurses dont have to create their own documentation framework for each patient or try to recall specific data points required by regulations. A template provides a clear roadmap, guiding them through the necessary fields and prompts. This not only speeds up the documentation process but also reduces cognitive load, allowing nurses to dedicate more mental energy to critical thinking and direct patient interaction, ultimately leading to higher job satisfaction and improved patient outcomes.
A truly effective documentation template also serves as a powerful tool for quality improvement initiatives. By standardizing the collection of data, healthcare organizations can easily aggregate and analyze information to identify trends, evaluate the effectiveness of interventions, and pinpoint areas for improvement in care delivery. This data-driven approach fosters a culture of continuous learning and refinement, ensuring that services provided are not only compliant but also consistently high-quality and evidence-based.
Key Elements to Include in Your Template
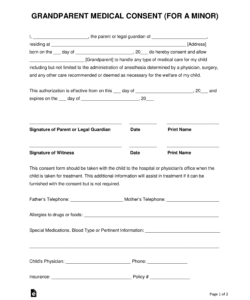
- Patient Demographics and Identification: Full name, date of birth, Medicaid ID, contact information.
- Initial Assessment: Comprehensive physical, psychosocial, and functional assessment data.
- Nursing Diagnosis and Problem List: Identification of actual or potential health problems.
- Individualized Care Plan: Specific goals, interventions, and expected outcomes tailored to the patient.
- Medication Administration Record (MAR): Details of all medications, dosages, routes, times, and nurse’s signature.
- Vital Signs and Physiological Monitoring: Regular readings and observations.
- Interventions and Treatments: Detailed records of all nursing actions, wound care, therapies, etc.
- Patient Response and Outcomes: Documentation of the patient’s reaction to interventions and progress toward goals.
- Education Provided: Information shared with the patient and family regarding their condition and care.
- Communication Logs: Records of discussions with other healthcare providers, family, or external agencies.
- Changes in Condition and Incident Reports: Prompt documentation of any significant changes or adverse events.
- Nurse’s Signature and Credentials: Ensuring accountability for all entries.
Designing and Implementing Your Ideal Medicaid Nursing Documentation Form Template
Creating a truly effective medicaid nursing documentation form template requires careful consideration of your specific practice setting and the unique needs of your patient population. While a generic template can provide a starting point, the most beneficial forms are those that have been customized to align with your organizations workflows, software systems, and the specific services you provide. Involving nurses and other direct care providers in the design process is invaluable, as their real-world experience can highlight practical considerations and ensure the template is user-friendly and comprehensive.
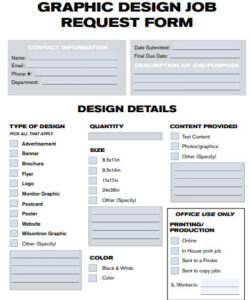
When designing your template, think about the logical flow of information. It should mirror the nursing process, moving from assessment to planning, intervention, and evaluation. Use clear, concise language and avoid jargon where possible. Incorporate checkboxes for common observations or actions to expedite documentation, but always leave ample space for narrative notes to capture the nuanced details that make each patient’s situation unique. The layout should be intuitive, guiding the nurse seamlessly through each required section without unnecessary complexity.
Considering whether to implement a paper-based or electronic template is another crucial decision. While paper forms are easy to print and distribute, electronic templates offer significant advantages in terms of accessibility, data integrity, and analytical capabilities. Digital forms can often be integrated with existing electronic health record (EHR) systems, automating data entry, reducing transcription errors, and allowing for real-time updates and secure data storage. The ability to quickly search, filter, and generate reports from electronic data can revolutionize how you manage patient information and identify trends.
Successful implementation of any new documentation template hinges on comprehensive training and ongoing support for your nursing staff. Even the most perfectly designed form will fall short if staff members are unsure how to use it correctly or inconsistently apply it. Provide clear guidelines, conduct hands-on training sessions, and offer accessible resources for questions. Encourage feedback from staff during the initial rollout phase to identify any unforeseen challenges or areas for improvement, fostering a sense of ownership and ensuring widespread adoption.
A well-designed and consistently used documentation template is more than just a piece of paper or a digital screen; it is a critical tool that underpins the delivery of high-quality, compliant care within the intricate Medicaid system. It empowers nursing professionals to work more efficiently, ensures that every aspect of patient care is meticulously recorded, and provides a clear, defensible record that stands up to scrutiny. By standardizing documentation practices, healthcare organizations foster a culture of accuracy, transparency, and accountability, which ultimately benefits both caregivers and the individuals they serve.
Embracing a systematic approach to nursing documentation, supported by robust templates, allows healthcare providers to navigate regulatory landscapes with confidence and optimize their operational efficiency. It means less time spent on administrative burdens and more time dedicated to compassionate, patient-centered care. The continuous refinement of these tools, based on evolving regulations and practical feedback, ensures that nursing documentation remains a dynamic and effective component of an excellent healthcare system.