In the dynamic world of medical education, ensuring the highest quality of teaching isn’t just a goal; it’s a necessity. The skills and knowledge imparted to aspiring doctors and healthcare professionals directly impact patient care and public health. This is where effective evaluation comes into play, serving as a crucial tool for improvement and excellence.
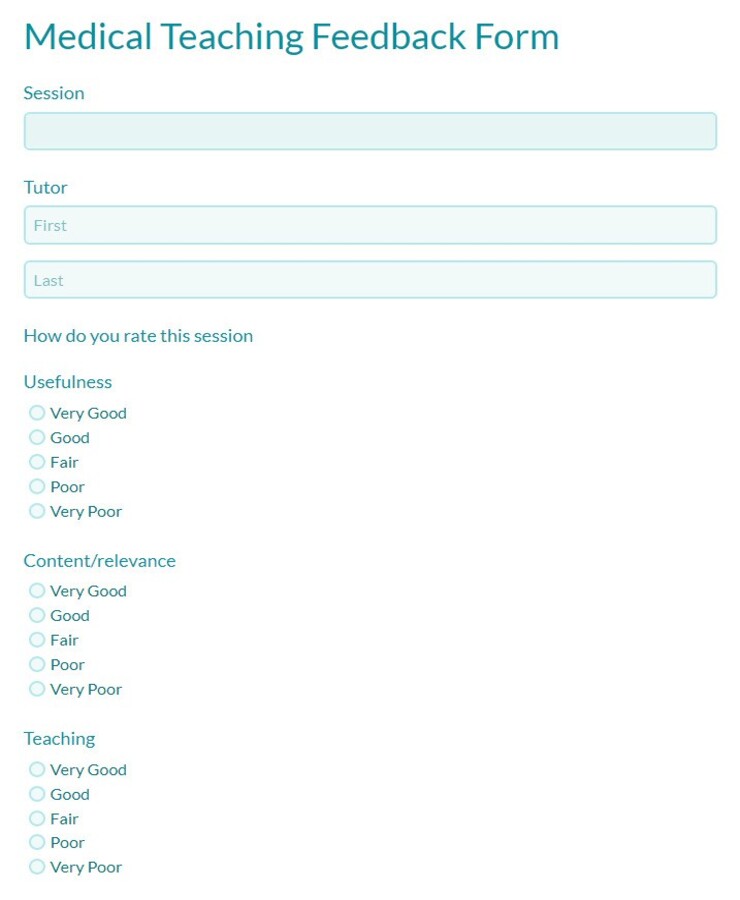
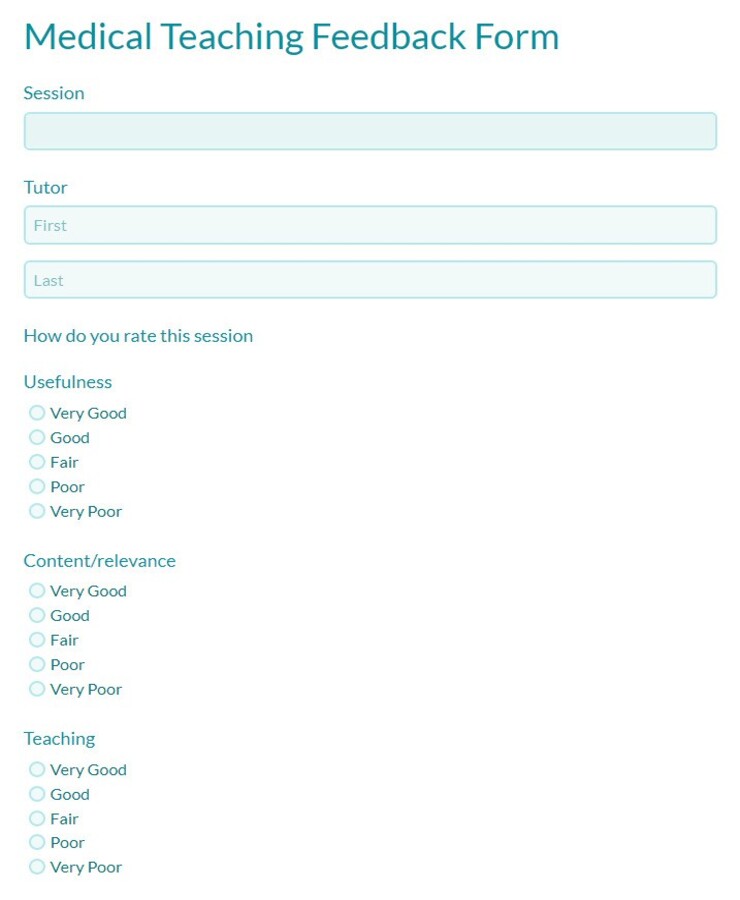
But how do we effectively measure and provide feedback on teaching performance in such a complex field? The answer often lies in structured, thoughtful assessment. A well-designed evaluation form provides a standardized way to gather insights, highlight strengths, and identify areas for growth, ultimately contributing to a richer learning experience for everyone involved.
Crafting an Impactful Evaluation Tool for Medical Teaching
Developing an evaluation system that truly captures the nuances of medical teaching can be challenging. It’s not enough to simply ask if a lecturer was “good.” We need a more granular approach that delves into various aspects of instruction, engagement, and content delivery. A comprehensive medical teaching evaluation form template can be an invaluable asset in this endeavor, providing a framework that ensures all critical areas are considered.
When creating or customizing such a template, think about the multifaceted role of a medical educator. They are not just delivering information; they are mentors, facilitators of critical thinking, and role models. Therefore, the evaluation should reflect this complexity, moving beyond simple satisfaction ratings to capture qualitative and actionable feedback.
Consider including sections that assess pedagogical skills, content expertise, and the learning environment. This allows for a holistic view of the teaching process. For instance, evaluating how well an educator structures their lectures, their ability to foster an interactive environment, or their commitment to providing timely and constructive feedback are all vital components.
A good template should also be adaptable enough to suit different teaching formats, whether it’s a large lecture, a small group tutorial, clinical bedside teaching, or a simulation exercise. The metrics for evaluating a surgeon teaching residents in an operating theatre might differ slightly from those for a professor delivering a pharmacology lecture, but the core principles of effective teaching remain constant.
Key Components of an Effective Medical Teaching Evaluation Form
- Clarity of Learning Objectives: Did the instructor clearly state what students were expected to learn?
- Content Expertise and Accuracy: Was the information presented accurate, up-to-date, and relevant?
- Teaching Methods and Engagement: Did the instructor use varied and effective teaching techniques? Did they encourage participation and critical thinking?
- Communication and Interpersonal Skills: Was the instructor approachable, clear in their explanations, and respectful?
- Feedback and Assessment: Did the instructor provide timely, constructive, and fair feedback on assignments or performance?
- Organization and Time Management: Was the session well-organized and did it adhere to the planned schedule?
- Overall Effectiveness: An overall rating of the instructor’s teaching performance.
- Open-Ended Comments: Space for detailed qualitative feedback, suggestions for improvement, and highlights of positive experiences.
Maximizing the Impact of Your Evaluation Forms in Medical Education
Having a robust medical teaching evaluation form template is only the first step. The true value comes from how these forms are implemented, processed, and, most importantly, acted upon. It’s about establishing a feedback loop that genuinely drives improvement, rather than simply collecting data for data’s sake.
Effective implementation involves thoughtful planning. Decide on the frequency of evaluations – perhaps after each major module, at the end of a rotation, or at specific points in the academic year. Ensure that students understand the purpose of these evaluations and that their input is genuinely valued. Anonymity is key to encouraging honest and constructive feedback. If students fear repercussions, even subtle ones, the quality of the feedback will suffer.
Once collected, the data must be systematically reviewed. This isn’t just a task for administrative staff; faculty leaders and the instructors themselves should be involved in analyzing the feedback. Look for patterns, recurring themes, and actionable insights. Is a particular teaching method consistently rated highly? Are there common areas where students feel less supported or confused?
The most critical step is translating these insights into tangible improvements. This could involve providing professional development opportunities for instructors, redesigning parts of the curriculum based on student feedback, or offering one-on-one coaching for educators. It’s about fostering a culture of continuous improvement where educators feel supported in their growth, not just judged.
Ultimately, a well-utilized evaluation system contributes significantly to the overall quality of medical education. It empowers students by giving them a voice, and it empowers educators by providing clear pathways for development. This symbiotic relationship ensures that future generations of healthcare professionals are taught by the best, equipped with the knowledge and skills necessary to navigate the complex world of medicine.
- Communicate the Purpose: Explain why evaluations are important for improving education.
- Ensure Anonymity: Use systems that protect student identity to encourage honest feedback.
- Regular Review: Schedule consistent times for faculty and administrators to review feedback.
- Provide Constructive Feedback: Share results with instructors in a supportive, growth-oriented manner.
- Action Planning: Develop clear plans based on feedback for curriculum adjustments or professional development.
- Close the Loop: Inform students and faculty about how their feedback led to improvements, reinforcing the value of the process.
Implementing a structured approach to assessing medical teaching is more than just an administrative task; it’s a commitment to excellence in healthcare education. By thoughtfully designing and consistently utilizing robust evaluation tools, educational institutions can foster an environment where teaching quality continually evolves and improves.
This dedication to refining teaching methodologies directly impacts the caliber of medical professionals entering the field. It ensures that students receive the most effective instruction, preparing them not only with vast knowledge but also with the critical thinking and practical skills vital for compassionate and competent patient care in the future.


