In the demanding world of medicine, where lives are literally in the balance, effective teaching is not just beneficial; it’s absolutely critical. Medical educators, whether they are seasoned professors, busy residents, or experienced clinicians, pour their knowledge and expertise into shaping the next generation of healthcare professionals. But how do we ensure that this teaching is truly hitting the mark, fostering deep understanding, and preparing students for real-world challenges? The answer, very often, lies in robust, constructive feedback. It is the compass that guides educators to refine their methods and students to optimize their learning.
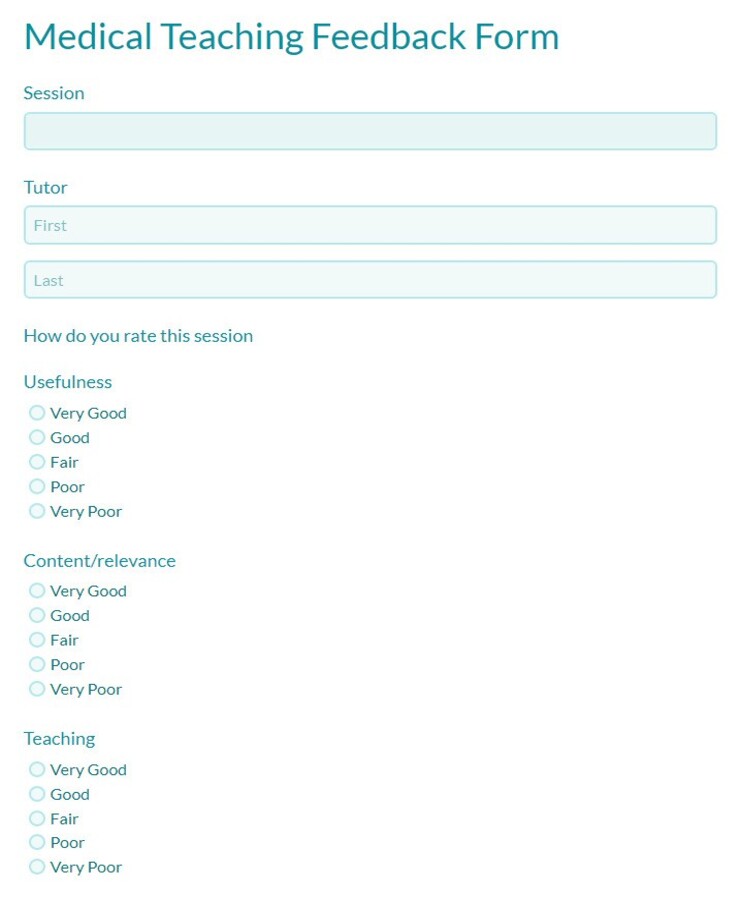
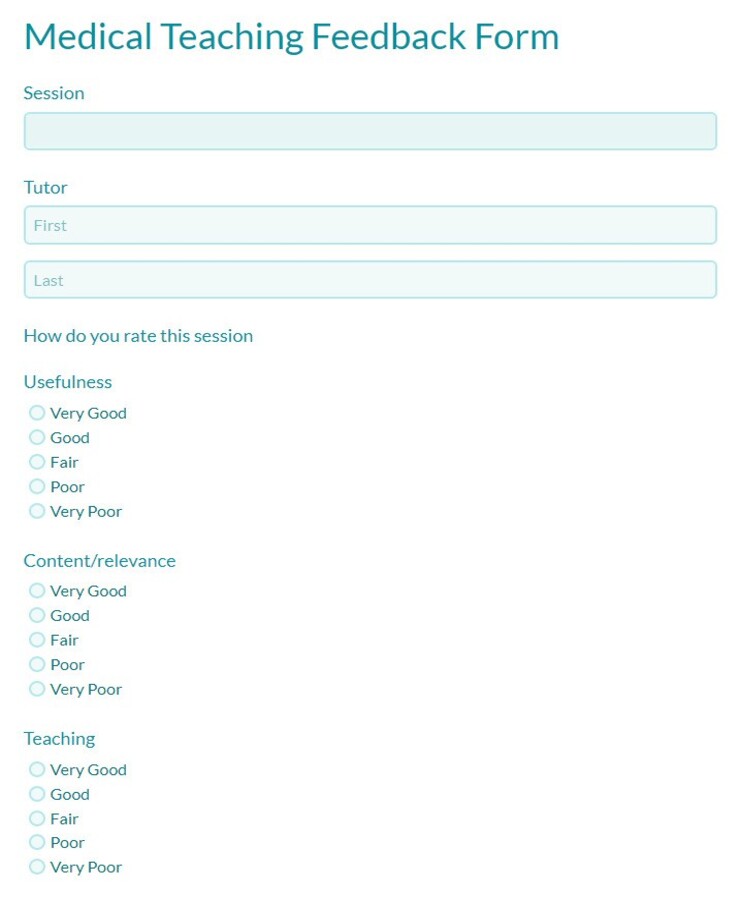
Gathering feedback, however, isn’t always straightforward. It requires a systematic approach to be truly valuable and actionable. Without a structured framework, feedback can be vague, inconsistent, or simply missed altogether. This is precisely why having a well-designed medical teaching feedback form template becomes an invaluable tool. It standardizes the process, encourages thoughtful responses, and provides educators with the specific insights they need to continually improve their craft.
Why a Dedicated Medical Teaching Feedback Form Template is a Game-Changer
Think about the sheer complexity of medical education. It’s not just about memorizing facts; it’s about developing critical thinking, clinical reasoning, communication skills, and empathy. For educators to effectively teach such a multi-faceted discipline, they need more than just general praise or criticism. They need detailed, specific input on what worked, what didn’t, and why. A dedicated template ensures that all key areas of teaching are consistently evaluated, providing a comprehensive picture.
Such a template moves beyond casual comments, turning subjective impressions into actionable data. It helps identify strengths to be leveraged and areas needing improvement, from the clarity of lectures to the effectiveness of clinical supervision. This systematic collection of feedback is crucial for professional development, allowing medical teachers to continually enhance their pedagogical techniques and adapt to the evolving needs of their learners and the healthcare landscape.
Furthermore, a well-structured feedback form empowers learners. It gives them a voice and a clear avenue to express their perspectives in a constructive manner. When students know their feedback is valued and will be considered, they become more engaged in the learning process itself, fostering a culture of mutual respect and continuous improvement within the educational environment.
Key Elements to Include in Your Template
When designing or choosing a medical teaching feedback form template, certain components are vital to ensure it captures comprehensive and useful data. Consider including sections that address:
By incorporating these elements, a template provides a holistic view of the teaching experience, enabling educators to make targeted adjustments for future sessions.
Crafting Your Own Effective Medical Teaching Feedback Form Template
While a general template provides a great starting point, the most effective medical teaching feedback form template is often one that’s been thoughtfully adapted to your specific context. Medical education varies widely across specialties, levels (undergraduate, postgraduate, continuing medical education), and teaching modalities (lectures, small groups, bedside teaching, simulation). Therefore, a one-size-fits-all approach might miss crucial nuances relevant to your particular setting.
Begin by considering your audience. Are you collecting feedback from medical students, residents, fellows, or even peer educators? Each group might have different perspectives and areas of focus. For instance, residents might be more attuned to mentorship and supervision quality, while early medical students might prioritize clarity of basic concepts. Tailoring the questions to the specific learning stage and objectives will yield more pertinent insights.
It’s also essential to strike a balance between quantitative (e.g., Likert scales for agreement) and qualitative (open-ended questions) feedback. While numerical ratings can quickly show trends and allow for easy comparison, the narrative comments are where the real gems of insight often lie. They provide context, specific examples, and suggestions that numerical ratings simply cannot convey. Encourage thoughtful, detailed responses in these open sections.
Finally, think about the practicalities of implementation. Will the form be anonymous to encourage candid responses? How often will feedback be collected? What is the process for reviewing the feedback and, crucially, acting upon it? Communicating to learners how their feedback will be used fosters trust and increases the likelihood of receiving valuable input in the future. The ultimate goal isn’t just to collect data, but to use it as a catalyst for meaningful improvement and to cultivate a culture of continuous learning and growth for everyone involved in medical education.
The continuous evolution of medical knowledge and practice means that educators must also continuously evolve their teaching methods. Implementing a robust system for collecting and acting on feedback is not just a good practice; it’s an essential component of delivering high-quality medical education. By consistently refining teaching approaches based on thoughtful input, we ensure that future healthcare professionals are equipped with the best possible foundation for their demanding and vital careers.


