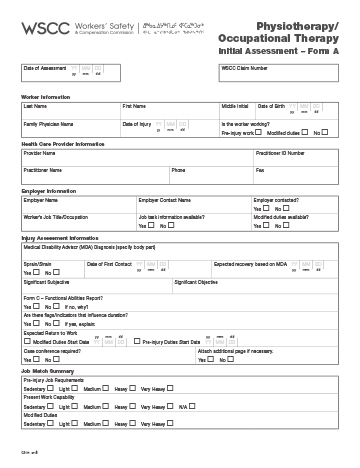
Stepping into a physiotherapy clinic for the first time can be a mix of hope and trepidation for patients. For physiotherapists, that initial encounter is a crucial opportunity to gather vital information, build rapport, and lay the groundwork for effective treatment. A well-designed initial assessment form isn’t just a piece of paper; it’s the very backbone of a thorough evaluation, ensuring no critical detail is overlooked and setting the stage for a successful recovery journey.
Understanding the patient’s history, current symptoms, lifestyle, and goals is paramount to formulating a personalized and effective treatment plan. Without a structured approach, important information might be missed, leading to less optimal care. This is where a comprehensive physiotherapy initial assessment form template becomes an invaluable tool, providing a systematic way to collect all necessary data, streamlining the intake process, and helping practitioners deliver the best possible care.
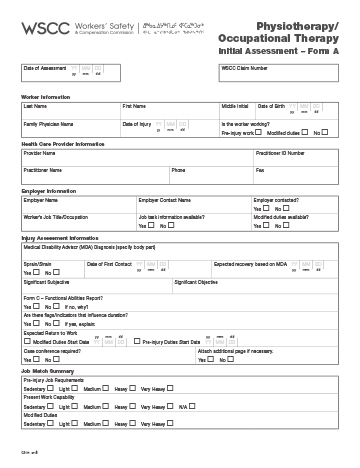
Key Components of an Effective Assessment Form
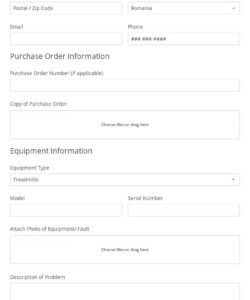
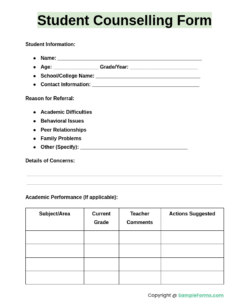
A robust physiotherapy initial assessment form template should be structured to capture a holistic view of the patient’s condition and needs. It begins with the basics, like contact information and demographics, ensuring you can communicate effectively and maintain accurate records. Beyond that, it delves into the specifics of their health, providing a detailed narrative of their journey to your clinic.
One of the most critical sections is the chief complaint and history of present illness. This is where the patient articulates why they’re seeking help, describing the onset, duration, intensity, and aggravating or relieving factors of their symptoms. Understanding their pain scale, functional limitations, and how their condition impacts daily activities offers immense insight. This narrative helps the therapist understand the patient’s perspective and immediate concerns.
Furthermore, a comprehensive medical history is non-negotiable. This includes past surgeries, existing medical conditions like diabetes or heart disease, medications they are currently taking, allergies, and any relevant family history. These details can significantly influence treatment choices and alert the therapist to potential contraindications or precautions. Social history, covering occupation, hobbies, and activity levels, also provides context to their physical demands and lifestyle, which are vital for setting realistic rehabilitation goals.
Finally, the form should guide the objective assessment section, allowing for a structured recording of physical findings. This typically includes posture analysis, range of motion measurements, muscle strength testing, neurological screening, special tests, and palpation findings. Having dedicated spaces for these observations ensures consistency across patients and allows for easy tracking of progress over time.
Essential Data Points to Include:
- Patient Demographics: Name, contact details, date of birth, emergency contact.
- Chief Complaint: Primary reason for visit, symptom description, onset, duration, previous treatments.
- Medical History: Past medical conditions, surgeries, medications, allergies, family history.
- Social History: Occupation, hobbies, lifestyle, functional limitations.
- Goals: Patient’s personal goals for therapy.
- Objective Assessment Findings: Range of motion, strength, palpation, special tests, posture.
- Treatment Plan: Initial plan, prognosis, and expected outcomes.
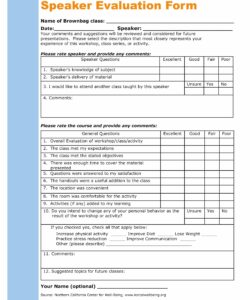
The Benefits of Standardizing Your Intake Process
Utilizing a standardized physiotherapy initial assessment form template offers numerous advantages for both the practitioner and the patient. For clinics, it creates consistency across all assessments, ensuring that every physiotherapist collects the same essential information. This not only streamlines the intake process but also facilitates better communication among team members if a case needs to be discussed or transferred.
Beyond consistency, efficiency is a major win. With a clear template, therapists can methodically go through each section, reducing the chances of forgetting key questions or repeating information. This saves valuable time during the initial consultation, allowing more focus on the physical examination and initial treatment, ultimately enhancing the patient experience by making the process feel organized and professional.
From a legal and administrative perspective, a well-documented assessment form is invaluable. It serves as a comprehensive record of the patient’s condition at the outset of treatment, offering protection in cases of disputes or audits. Furthermore, it aids in justifying the necessity of treatment to insurance companies and provides a solid foundation for progress notes and discharge summaries.
Ultimately, a robust physiotherapy initial assessment form template contributes directly to improved patient care. By ensuring all relevant information is captured upfront, therapists can develop more precise, individualized treatment plans. It empowers practitioners to make informed decisions, track progress effectively, and ultimately guide patients more efficiently towards their recovery goals, leading to better outcomes and higher patient satisfaction.
Implementing a comprehensive assessment form ensures every patient receives a thorough evaluation from their very first visit. It transforms a potentially chaotic information-gathering session into a structured, professional interaction that benefits all parties involved. By carefully documenting all aspects of a patient’s condition and history, clinics establish a strong foundation for effective treatment plans.
A well-designed form is more than just paperwork; it’s a critical tool that supports clinical decision-making, enhances communication, and contributes significantly to the overall quality of care delivered. Embracing a standardized approach to initial assessments sets the stage for success, fostering better patient outcomes and a more efficient practice.