Making decisions about your own healthcare is a fundamental right, and it is something many people take very seriously. While we often focus on the consent aspect – agreeing to treatments – there’s an equally important side: the right to refuse care. This might stem from personal beliefs, a desire to avoid certain risks, or simply preferring an alternative approach. Understanding how to properly document such a decision is crucial for both patients and healthcare providers, ensuring everyone’s wishes and responsibilities are clear.
Proper documentation isn’t just a formality; it serves as a vital record, preventing misunderstandings and protecting all parties involved. When a patient decides against a recommended medical intervention, having a clear, legally sound document can make a world of difference. It ensures that the patient’s informed choice is respected and that healthcare professionals have a record demonstrating they communicated all necessary information.
Understanding Your Right to Refuse Care and Why a Form Matters
Your autonomy in healthcare means you have the power to accept or decline medical interventions, even if that decision might go against medical advice. This principle of informed refusal is as important as informed consent. Healthcare providers are ethically and legally bound to respect these decisions, provided the patient has the mental capacity to understand the implications of their choice. However, for this right to be fully effective and for all parties to be protected, proper documentation is absolutely essential.
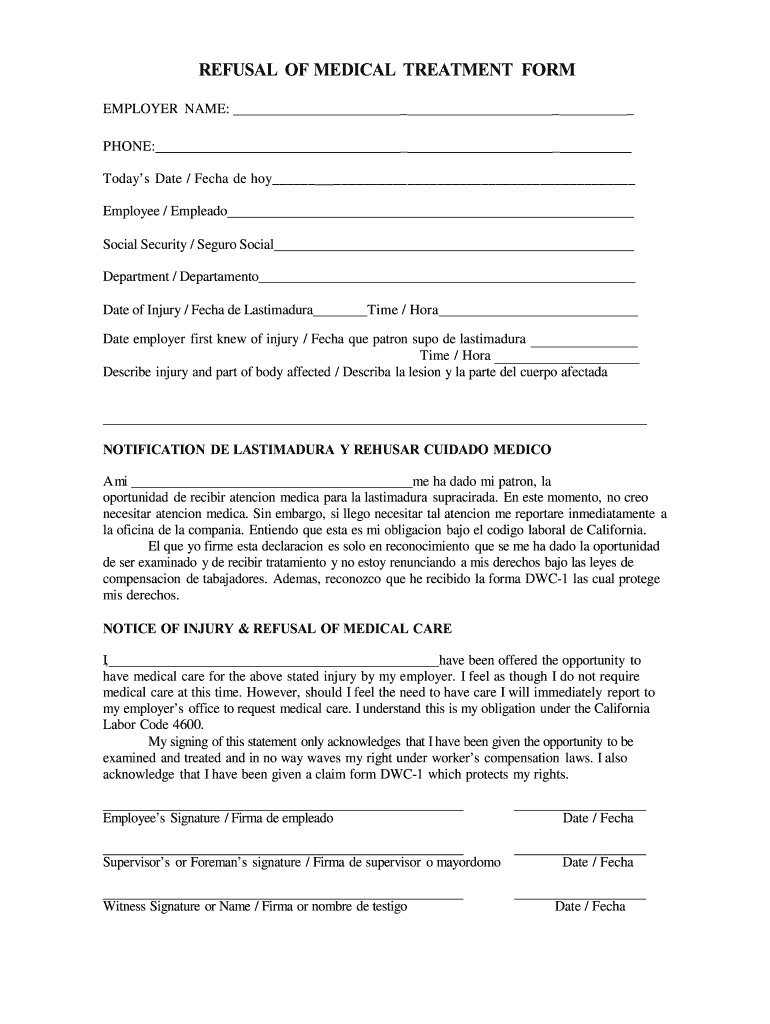
Imagine a situation where a patient clearly states they do not wish to undergo a specific surgery. Without a formal record, it could become a "he said, she said" scenario, potentially leading to disputes or misinterpretations down the line. A refusal of medical treatment form template serves as that official record, detailing the conversation, the risks explained, and the patient’s clear decision. It protects the healthcare facility from claims of negligence and protects the patient by ensuring their wishes are undeniably recorded.
Key Components of a Robust Refusal Form
A comprehensive refusal form isn’t just a blank piece of paper; it’s a structured document designed to capture all critical information. When considering or using such a template, look for sections that address:
- Patient identification details: Full name, date of birth, contact information.
- Specific treatment being refused: Clearly identifying the procedure, medication, or intervention.
- Acknowledgement of risks: A statement confirming that the patient understands the potential consequences and risks of refusing the treatment, as explained by the healthcare provider.
- Acknowledgement of alternatives: If applicable, a note that alternative treatments or palliative care options were discussed.
- Patient’s statement: A section where the patient explicitly states their decision to refuse and that they are doing so voluntarily.
- Provider’s attestation: A part for the healthcare professional to confirm they explained the treatment, risks, and alternatives, and believe the patient understood.
- Signatures: Spaces for the patient’s signature, the healthcare provider’s signature, and typically, a witness signature.
- Date and time: Crucial for establishing the exact moment the decision was documented.
This detailed approach ensures that the refusal is genuinely informed and that the patient’s best interests, as they define them, are upheld. It’s not about forcing anyone, but about ensuring clarity and respect for individual choice within the medical framework.
Navigating the Process: When and How to Use the Template
The use of a refusal of medical treatment form template typically arises after a thorough discussion between a patient and their healthcare provider. It’s not the first step in care, but rather a necessary measure when a patient, after understanding all aspects, decides against a recommended course of action. This might occur in various settings, from a routine clinic visit to a hospital emergency room, whenever a patient with capacity declines a specific treatment.
The process usually involves several key stages. First, the healthcare provider must ensure they have clearly explained the proposed treatment, its benefits, potential risks, and any available alternatives, as well as the risks of refusing the treatment. This is not just a quick chat; it’s an in-depth conversation tailored to the patient’s understanding. If, after this comprehensive discussion, the patient still chooses to refuse, that’s when the formal documentation becomes vital.
- Informed Discussion: The healthcare provider outlines the medical recommendation, explaining why it’s beneficial and what risks are associated with it.
- Understanding Risks of Refusal: Crucially, the potential negative health outcomes of declining the treatment are thoroughly explained and understood by the patient.
- Documentation: The refusal of medical treatment form template is then presented. The patient reviews the document, confirming it accurately reflects their understanding and decision.
- Signatures: The patient signs the form, often in the presence of the healthcare provider and a witness, affirming their voluntary and informed refusal.
- Medical Record: The completed form is then added to the patient’s permanent medical record, serving as an official account of the event.
It’s important to remember that these forms are not intended to coerce or intimidate patients. Instead, they are tools to facilitate clear communication and protect the rights and responsibilities of both patients and providers. They signify a moment where a patient’s autonomy is exercised and formally acknowledged, ensuring that their healthcare journey remains aligned with their personal wishes.
Having a clear process for documenting refusal of medical treatment is invaluable. It ensures that your personal healthcare decisions are not only heard but also formally respected within the medical system. This clarity provides peace of mind for you and your family, knowing that your choices regarding your body and health are meticulously recorded. It also protects healthcare professionals, demonstrating due diligence and adherence to ethical guidelines. Ultimately, such documentation strengthens the patient-provider relationship by fostering transparency and mutual respect, ensuring that your healthcare journey reflects your authentic wishes, even when they diverge from typical medical advice.