In healthcare, patient safety is the absolute top priority. Unfortunately, even with the most dedicated teams and best intentions, serious unexpected events, often called “sentinel events,” can occur. These incidents, which result in death, serious physical or psychological injury, or the risk thereof, demand immediate and thorough investigation. They’re not just unfortunate occurrences; they’re critical learning opportunities that can prevent future harm and significantly improve patient care.
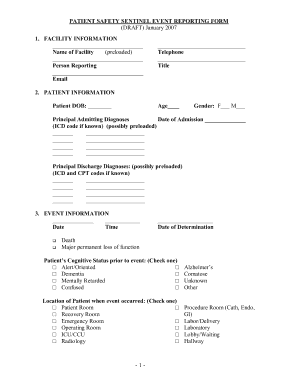
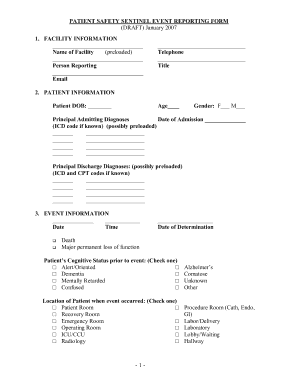
Understanding why these events happen is key to preventing their recurrence. That’s where a structured approach comes into play. A well-designed sentinel event analysis form template becomes an indispensable tool for healthcare organizations. It provides a systematic framework for investigation, ensuring all critical aspects of an incident are thoroughly examined, root causes are identified, and effective preventative measures are put in place. It’s about moving beyond blame and focusing on systemic improvements.
Understanding the Core of Sentinel Event Analysis
When a sentinel event occurs, the immediate response is crucial, but the long-term benefit comes from a deep dive into “why.” This is the essence of sentinel event analysis. It’s a comprehensive, systematic review process that aims to identify the underlying factors that contributed to the event, rather than just focusing on the individual actions involved. The goal is to discover systemic vulnerabilities and implement changes that make the healthcare environment safer for everyone.
A well-crafted form template is more than just a document; it’s a guided pathway for this critical investigation. It standardizes the process across an organization, ensuring consistency and comprehensiveness, no matter who is conducting the analysis. This means every relevant piece of information, from the initial details of the event to the final corrective actions, is captured systematically.
Typically, a robust sentinel event analysis form template will guide you through several crucial stages of investigation. It prompts for detailed descriptions, encourages collaborative input from various departments, and ensures that the focus remains on process improvement rather than individual fault. This structured approach helps prevent crucial details from being overlooked, leading to more accurate root cause identification.
Think of it as building a puzzle. Each section of the template provides a piece of the puzzle, helping you to reconstruct the incident and understand the bigger picture of what went wrong and, more importantly, how to fix it. This systematic capture of data is vital for learning and making lasting improvements within the healthcare system.
Here are some common sections you’ll find in a comprehensive sentinel event analysis form template:
- Event Description: A detailed narrative of what happened, when, and where.
- Initial Response: Actions taken immediately after the event.
- Impact Assessment: The actual or potential harm to the patient and others.
- Investigation Team: Who was involved in the analysis process.
- Timeline of Events: A chronological breakdown leading up to and including the incident.
- Root Cause Analysis: Utilizing methods like the “5 Whys” or fishbone diagrams to uncover underlying system failures.
- Contributing Factors: Identifying environmental, human, and system factors.
- Action Plan Development: Specific, measurable, achievable, relevant, and time-bound (SMART) corrective actions.
- Implementation and Monitoring: How actions will be put into practice and tracked for effectiveness.
- Lessons Learned: Generalizable insights for organizational improvement.
Implementing and Maximizing Your Sentinel Event Analysis Form Template
Having a fantastic sentinel event analysis form template is one thing, but truly leveraging it for maximum benefit is another. It’s not just about filling out boxes; it’s about fostering a culture of continuous learning and safety within your organization. The template should serve as a dynamic tool that facilitates deep thought and collaborative problem-solving, rather than a mere checklist to be completed.
Effective implementation hinges on a few key factors. First, ensure that all staff members who might be involved in an investigation are properly trained on how to use the template. This includes understanding its purpose, the meaning behind each section, and the importance of thorough and objective documentation. Training helps standardize the quality of data collected and the depth of analysis performed.
Secondly, encourage a multidisciplinary approach to investigations. Sentinel events rarely stem from a single cause or department. Bringing together diverse perspectives – clinical staff, administrators, quality improvement specialists, and even IT personnel – can uncover insights that a singular viewpoint might miss. The template should be a shared space where these different voices can contribute to a comprehensive understanding of the event.
Furthermore, the utility of the template extends far beyond the initial investigation. It’s a living document that informs subsequent actions. Once corrective measures are identified and implemented, the template can be used to track their effectiveness over time. Regular reviews of completed forms, perhaps monthly or quarterly, can reveal recurring themes or persistent vulnerabilities that require broader, systemic interventions.
Ultimately, a well-utilized sentinel event analysis form template is a cornerstone of a proactive patient safety program. It empowers organizations to learn from adverse events, transform those lessons into actionable improvements, and systematically reduce the risk of future harm. It cultivates an environment where safety is everyone’s responsibility and continuous improvement is the norm, leading to better outcomes for patients and a more resilient healthcare system overall.
Here are some tips for making the most of your template:
- Regular Training: Ensure all relevant staff understand how to accurately and thoroughly complete the form.
- Foster a Just Culture: Emphasize that the analysis is about system improvement, not individual blame.
- Multidisciplinary Teams: Involve diverse perspectives in the investigation process.
- Actionable Outcomes: Ensure that every identified root cause leads to a specific, measurable corrective action.
- Follow-Up and Monitoring: Implement a system to track the effectiveness of corrective actions.
- Share Lessons Learned: Disseminate insights and recommendations across the organization to prevent similar incidents.
- Regular Review: Periodically assess the template itself to ensure it remains relevant and effective.
Investigating and learning from adverse events is not merely a regulatory requirement; it’s a fundamental commitment to providing the highest quality of care. By meticulously analyzing what went wrong, healthcare organizations can transform potential tragedies into powerful catalysts for change and innovation. This diligent process ensures that every patient interaction contributes to a continually improving and safer environment.
Embracing a systematic approach to incident analysis builds a more resilient and responsive healthcare system. It cultivates a culture where continuous learning is paramount, errors are seen as opportunities for growth, and patient safety is woven into the very fabric of daily operations, ultimately benefiting everyone involved in the care continuum.


